When it comes to authorization management in healthcare industries, it’s a long-drone process that undergoes a series of steps before the ball gets rolling. Administrative tasks have always been a heavy burden that acts as a bottleneck in the healthcare system, particularly since the process eats up precious time before reaching the final intent.
Tracking the workflow itself is a confusing ordeal as it requires staff to arduously go through multiple data entries, payer rule discrepancies, and documentation that run the risk of having data inconsistencies.
Everything can lead to treatment delays and negatively impact patient outcomes, but the medical industry needs to streamline the authorization process is now a necessity as the COVID-19 outbreak demands more efficient planning to meet the rising number of coronavirus cases.
An Overview of the Authorization System and the Pandemic
It’s easy to think that the healthcare industry isn’t losing revenue as it caters to national demand in light of the pandemic, but the American Hospital Association shows that hospitals and other health systems lost a whopping $202.6 billion in revenue from the start of the outbreak since March through June.
There’s an expected shortfall of $120.5 billion from July to the end of the month in 2020, pushing a significant number of hospitals into bankruptcy and cutting off people from access to quality healthcare in a time when it is paramount more than ever.
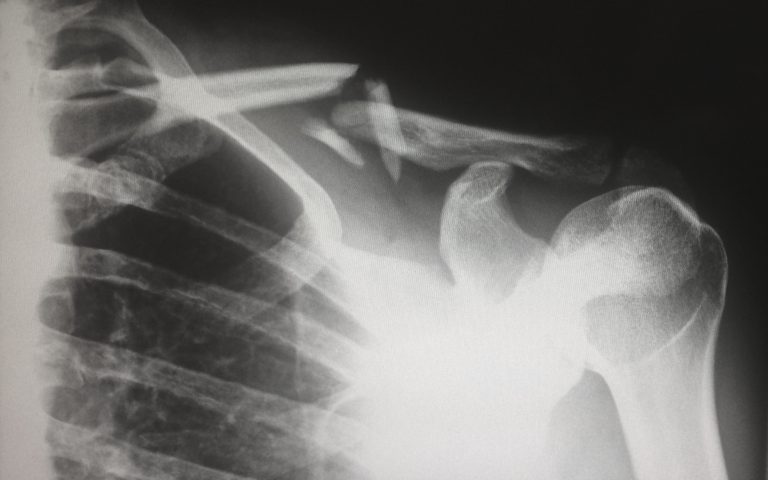
Part of the money lost is through prior authorization as it is the most time-consuming task in hospitals, compromising the productivity, and other resources, which translates to millions of dollars lost for the bottom line.
The Promise if Automating Prior Authorization
When it comes to prior authorization, the process starts with determining the patient’s needs, submitting the request, and then an authoritative figuring having the final say on its approval or denial.
Incorporating AI-powered technologies and automating the process can cut down a significant number of resources and time from prior authorizations, simplifying an otherwise convoluted administration task.
This means ensuring that automation technology is compatible with current medical records systems, removing errors and inconsistencies when transferring clinical and administrative information from one software to another.
Implementing a single access point should also take unnecessary steps out of the picture, allowing a cross-functional staff to access sensitive data and seamlessly sift through their tasks as efficiently as possible.
The Bottom Line: The Role of Automation in Addressing Efficiency Challenges in Healthcare Industries
The road to integrating automation to enhance prior authorization in the healthcare industry will be a long one, but it’s worth taking as studies show that it can reduce the burden and help the struggling industry to save as much as $25 billion annual healthcare costs.
Why Read Healthcare with Us?
Read more from our healthcare news site and stay in the loop to the latest trends and updates. Stay tuned for more health news today at Dose of Healthcare to keep your well-being in check!