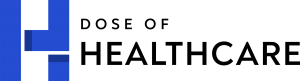
The global pandemic––Coronavirus––has caused millions of Americans to fall sick. Today, streets are emptied, and individuals are forced to stay inside their homes and practice social distancing in an attempt to curb the spread of this strain of the virus. Amidst the chaos that is happening, many Americans are fearsome of how much healthcare will cost them. In most cases, getting tested for coronavirus is free. Yet, many people still do not have access to the tests in the U.S., which adds to the delayed treatments.
There are people who have voiced out their concerns about their insurance company not covering the medical costs should they test positive for coronavirus. Nearly one in three families had decided not to get any medical care the past year because of the costs that they may incur, while three in ten people with medical expenses had to take out loans or tap into their savings to cover medical expenses.
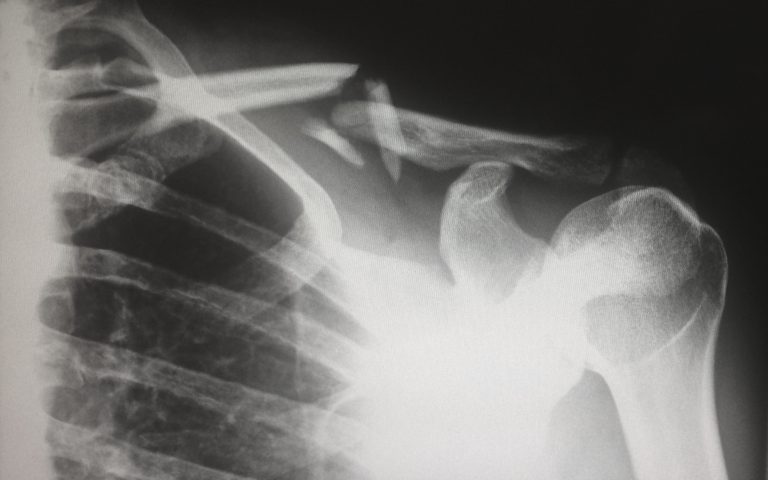
Patients Have to Cover Their Deductible
Health insurance providers cover coronavirus the way they cover similar illnesses. However, this also means that consumers will have to take care of their deductibles, which typically vary on the insurer and the plan.
Today, when individuals receive medical care for coronavirus, they will face additional costs in the form of deductible, co-pay, or co-insurance before the coverage kicks in. The same rule applies to individuals with a 10% copayment after the deductible. In this case, individuals will pay for 10% of any additional healthcare up to the yearly limit of the plan. Patients who were treated in a facility or doctor that is not within the network of the health insurance plan, on the other hand, may be presented with a huge bill.
Scott Flanders, CEO of eHealth (EHTH), said, “This happens more often than one might think and the magnitude of an out-of-network bill for COVID-19 care could be staggering. Some states have started to pass laws prohibiting it, since Congress has failed to do so. I do think that there will be public pressure for insurers, hospitals, and doctors to meet the need of Americans in this unusual moment without leaving them with unaffordable medical bills. Yes, it is a moment where the gaping holes in our health care financing system become glaringly obvious.”
Know that healthcare costs following the diagnosis of COVID-19 will be covered as long as it remains consistent with the standard provisions of the health benefits of the member. Furthermore, Blue Cross Blue Shield will waive prior authorization for necessary COVID-19 related medical and diagnosis services.
Quarantined Patients At Home
Individuals who will be quarantined in a medical facility need not worry because insurers will cover the medical costs during this period. However, there may be other costs that the patient has to shoulder with their own money.
In the case that you are forced to do a self-quarantine at home, your insurer will not pay you while you’re in home quarantine or compensate for your loss of income throughout the quarantine period. On the other hand, patients who are in-home quarantine but visit doctors for check-ups and tests will be covered by their health insurance plan.
If you want to stay updated, browse our website today for more news in the medical industry.