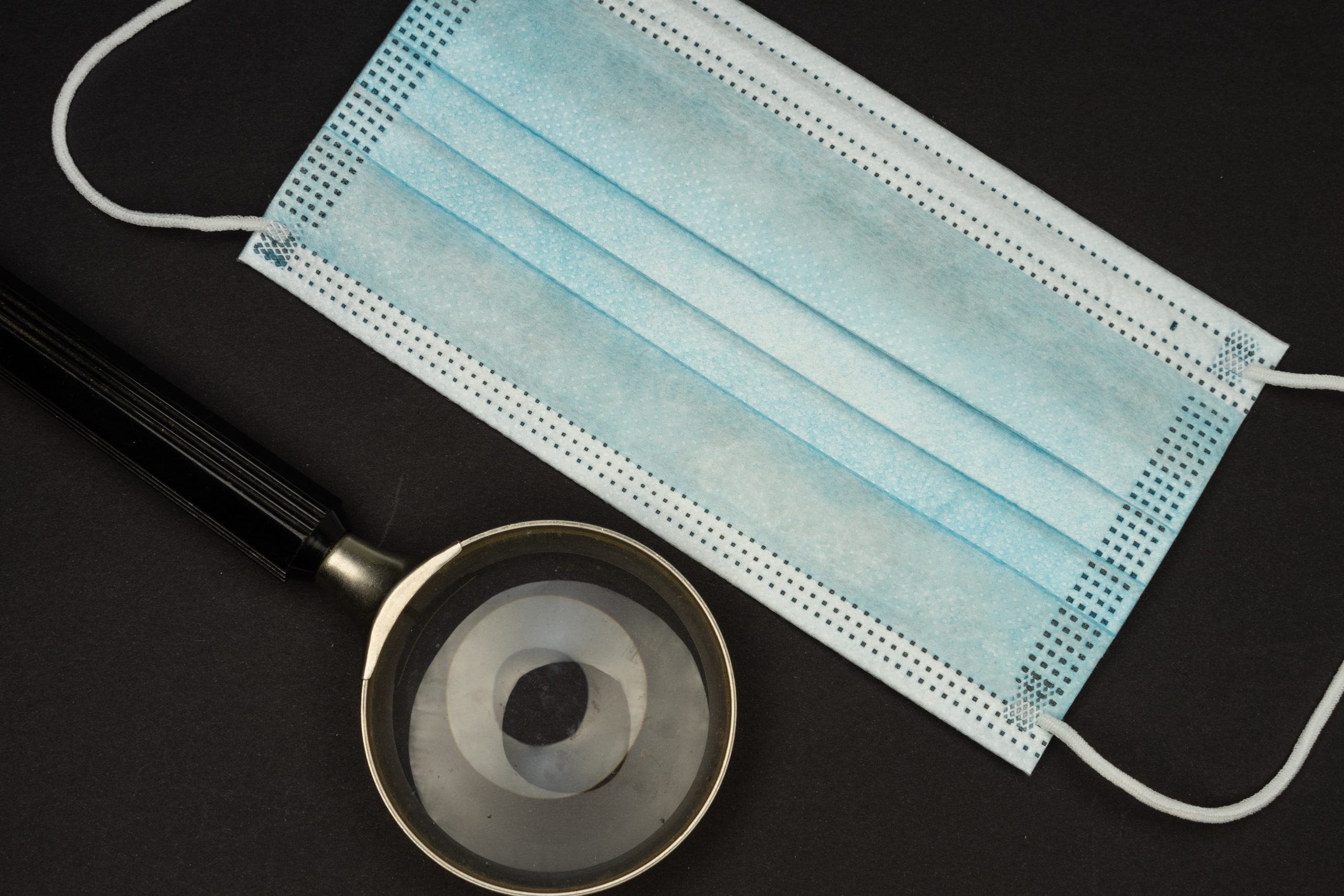
Most medical news in 2020 revolved around the coronavirus pandemic, and COVID-19 has affected everything about the medical industry today. For instance, post-acute care or PAC facilities had a very challenging 2020, mainly due to the outbreaks in skilled nursing facilities and the surge in need for home health and hospice care. Here are five likely scenarios the PAC sector will see in the coming years.
PAC Facilities Get Closer To Interoperability
Interoperability is the ability of various systems and applications to exchange and use data cooperatively. It aims to coordinate patient information across departments, facilities, and regional or national boundaries so that all involved facilities can provide optimal healthcare.
For years, various organizations have created a foundation for interoperability, making care transitions safer for the patient. PAC providers are reaping the initial benefits, and with increased data sharing and the refining of processes, interoperability will be a reality for the rest of the medical industry.
Consumer-Centric Healthcare Experiences
Today, service providers think about “user experience” like how corporations would, since patients today expect better healthcare experiences. Technology is also playing a large part in patient-centricity. Online, providers can create a digital presence that highlights their patient-first philosophy. Offline, innovations in tech enhance care delivery.
Payment Models Are Still A Significant Factor
Regulatory and financial factors will still be significant in the coming years. PAC providers can weather any changes, though, if they become proactive. By understanding payment models and their effects, learning from previous payment reforms, and choosing the best partners, a post-acute care facility can control its bottom line.
New Operations Processes For PAC Companies
PAC companies want to know how to deliver better patient outcomes and greater value at the same time. Because of the rise in home-based health care services, PAC facilities and organizations must find ways to retain patient share. Diversifying can help them reduce vulnerabilities in service.
Universal Healthcare Is Still Just Beyond Reach
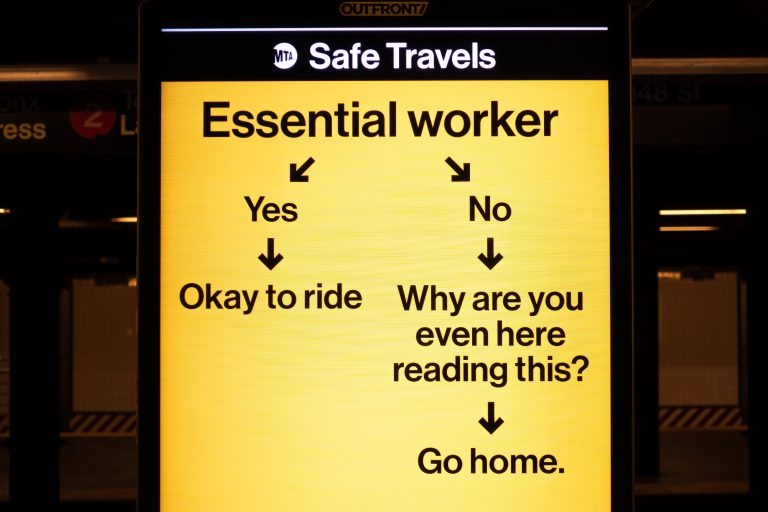
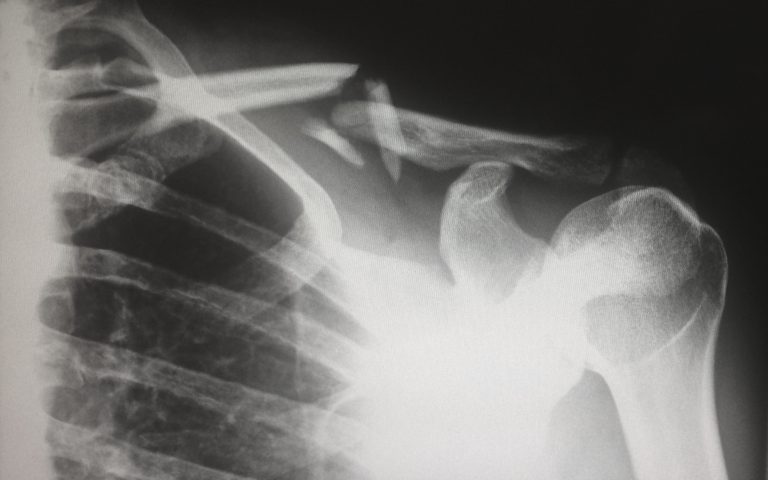
COVID-19 threw into high relief the structural inequities in the American healthcare system. Some places are moving towards equity. For example, a new national care program aims to reduce health outcome disparities for Black patients who had undergone hip and knee joint replacements.
The CMS Comprehensive Care for Joint Replacement model reduces spending and improves outcomes for all patients, and it is Black patients who benefit greatly from it. Under the new bundled payment model, Black patients have a decreased risk of readmission and stay in the hospital for roughly the same time as white and Hispanic patients.
However, this is only one program for one field in medicine. People need more programs for various specializations, especially in the wake of a global pandemic like COVID-19.
Conclusion
The COVID-19 health crisis was historic since it was both disruptive and unprecedented, upending systems and halting progress globally. For most of last year, healthcare professionals and facilities operated on an as-needed basis, reducing their planning capacity. In the new year, though, this reliance on contingencies cannot be par for the course. Healthcare organizations must have one eye on the future. These five trends offer a glimpse into what is to come.
For more health and medical news, keep reading Dose of Healthcare. We cover the latest developments and innovations in the public health industry—bookmark our page and never miss another story.