Imagine you’re required to undergo minor surgery. To prepare, you call your insurer way ahead of time to double-check that your hospital is “in-network” with your insurance. You even go out of your way to reach out to your doctor in charge if they are also in-network.
Confirming these things gives you peace of mind that you won’t get surprise charges after the procedure aside from your usual co-pay, but once you get your bill, the hospital blindsided you with a staggering bill that you have no idea how to get out of.
This hypothetical scenario, unfortunately, is not an example of an isolated case. According to a new study, one in five patients may receive a surprise medical bill after non-emergency surgeries like knee replacement or hysterectomy.
The latest issue of the Journal of the American Medical Association (JAMA), a peer-reviewed medical periodical, reveals that roughly 20 percent of common operations result in surprise bills, leaving patients with tens of thousands of dollars in unexpected charges despite having procedures done in in-network facilities by in-network surgeons.
The average unexpected charge was around $2,011 more than the $1,800 a privately insured patient would already have to spring for after their insurance has already paid for most of the costs involved in the operation. This can especially hurt people who have to deal with other health issues or those who experience complications after the initial surgery.
“Even if patients do their homework before they have elective surgery, this study shows they can be at risk of receiving large bills they never expected, from providers they never met or even knew about,” Dr. Karan Chhabra, the lead author of the University of Michigan study, said in a press release.
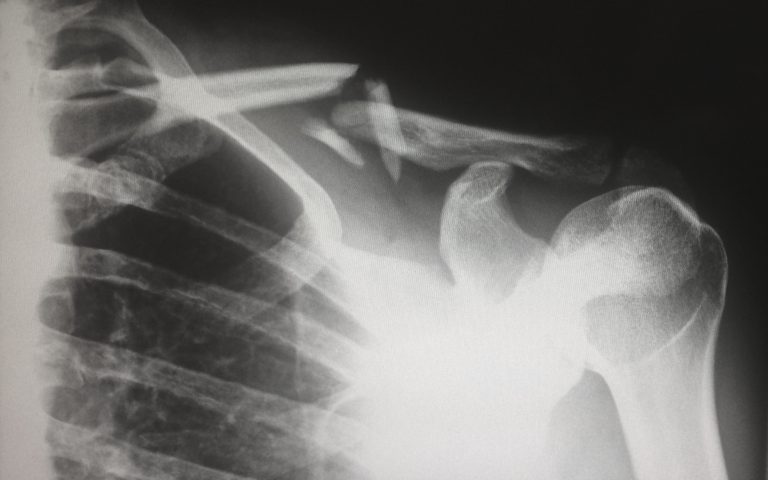
But what’s curious about all of this is that the surprise costs don’t come from the in-network hospital or surgeon. They originate from other medical staff at the facility involved in the procedure or aftercare who may not be part of the patient’s insurance network.
This may include anesthesiologists or surgical assistants who have had hands-on involvement during the surgery or postoperative care. In the study, the researches found out that they account for more than two-thirds of the unexpected charges.
With the involvement of other medical staff who are out of network, the average bill the patient might incur could be as high as $3,633. Other people who required more care may pay so much more.
It gets even worse if the patient underwent an outpatient procedure with an in-network surgeon at an ambulatory surgery center that was out-of-network. The surprise bill can skyrocket up to more than $19,000.
While there’s no comprehensive federal law in place to solve this just yet, patients can take the proactive approach and fully understand what their insurance covers. It also helps to speak with the doctor and ask to be referred to only specialists in the same network. And when push comes to shove, there’s always the option to fight the bill and file for an appeal.
Browse our website today for more news in the medical industry.